Breast cancer is the most common cause of cancer (excluding skin) in women, and the 2nd leading cause of cancer death in U.S.
An estimated 1 in 8 women in U.S. will be diagnosed with breast cancer.
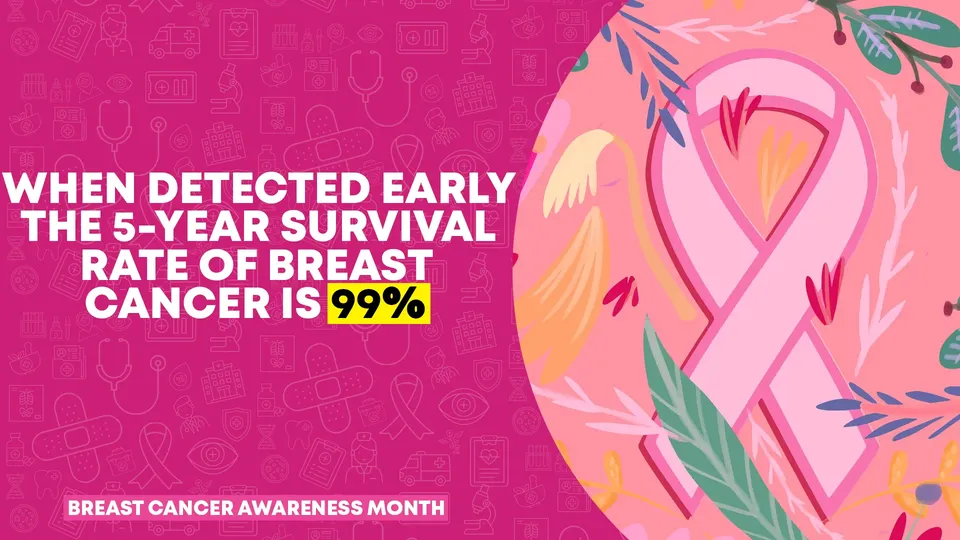
Similar to other diseases, we know that early detection greatly improves treatment options, availability, and success. This is why early detection of breast cancer through routine screenings is so important.
When to Start Screening
Starting at age 40-49 patients should have a discussion with their health care provider about starting or frequency of screening. For those placing greater value on prevention over risk, biennial screening should be considered (start biennial screening age 45).
This does not include patients with a greater risk due to family history of breast cancer, a known genetic mutation, or a history of chest radiation—where consultation should start at 25-35.

Types of Breast Cancer Screenings

Mammography
Xray study (radiation dose 0.4 millisieverts mSv—1/10 of the radiation flying East to West coast).

Ultrasound
No radiation, useful for further defining certain types of lesions (such as cysts).

Breast MRI
No radiation, but often only used in specific circumstances for women with certain risk factors.

Clinical Breast Exam (CBE)
In-office visit that may not be routinely recommended for screening due to high variability in exam findings.

Self breast exam (SBE)
Okay to do for awareness of change but not routinely recommended for screening due to lack of accuracy.
Thermography
No radiation. Usually only used in combination with other testing due to a lack of reliable studies showing early detection and inability to detect deeper lesions.
How Much of Impact do Screenings Make?
Best survival is related to earlier detection plus better follow-up medical care. Countries and populations with poorer screening options have worse 5 year survival rate — as low as 45% compared to over 90% in countries with increased screening.
Thus regular well visits and discussions with a health care provider pay significant dividends.